Re-imagining New York City's mental health emergency response
A new health-centered approach to mental health emergencies

B-HEARD - the Behavioral Health Emergency Assistance Response Division - is part of New York City's commitment to treat mental health crises as public health problems - not public safety issues. For the first time in New York City's history, teams of health professionals - including EMTs/paramedic from NYC Fire Department and mental health professionals from NYC Health + Hospitals - are responding to 911 mental health calls through a pilot program that launched in spring 2021.
Learn more about B-HEARD using the links below.
Social workers: Join the B-HEARD team!
B-HEARD at a glance
The latest news on B-HEARD
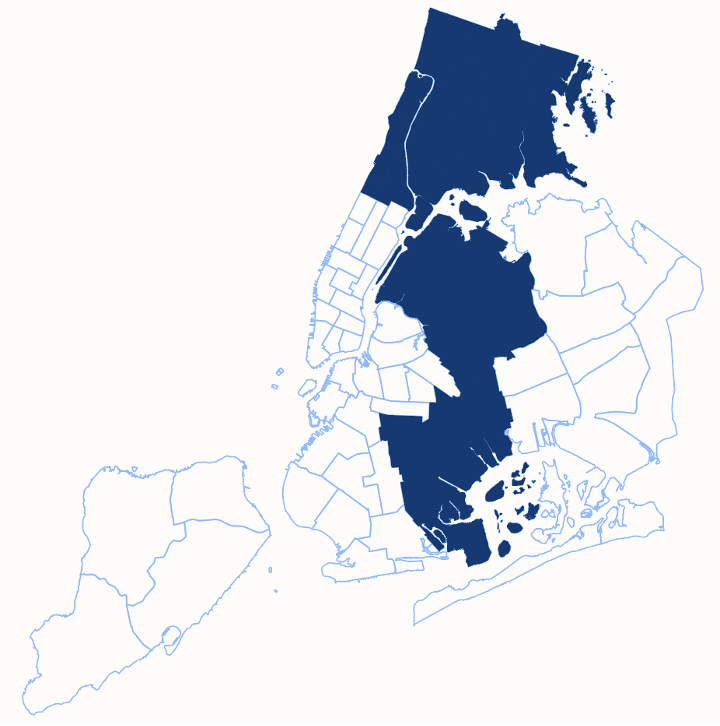
In November 2021, the B-HEARD pilot expanded to respond to 911 mental health calls from East Harlem to the Hudson River. In March 2022, the B-HEARD pilot expanded to Washington Heights, Inwood, and parts of the South Bronx. In June 2022, B-HEARD expanded to two additional police precincts in the South Bronx. In October 2022, B-HEARD expanded to the remainder of the South Bronx and to East New York and Brownsville. In March 2023, the Mayor announced the City’s commitment to expand B-HEARD citywide as part of his Mental Health Plan. That same month, B-HEARD expanded into parts of Queens for the first time, and additional neighborhoods in Brooklyn. In October 2023, B-HEARD expanded to cover the entire borough of the Bronx.
The City has made significant investments to strengthen mental health crisis prevention and response including and beyond the B-HEARD pilot.
Have a question about B-HEARD? Collapse and expand the FAQ below to learn more about the pilot.
The Behavioral Health Emergency Assistance Response Division, or B-HEARD, is a health-centered response to 911 mental health calls launched in June of 2021. Beginning with a pilot in Harlem, B-HEARD Teams — FDNY Emergency Medical Technicians (EMTs)/paramedics teamed with a mental health professional from NYC Health + Hospitals — are dispatched as first responders to people experiencing a mental health emergency. B-HEARD Teams operate seven days a week, 16 hours a day.
The B-HEARD Teams use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations and provide immediate care. These teams have the expertise to respond to a range of behavioral health problems, such as suicidal ideation, substance misuse, and mental health conditions, including serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. If the person requires emergency medical services, the EMTs or paramedics on the B-HEARD Team are able to provide emergency medical care and call for an ambulance transport. B-HEARD teams do not transport patients.
In emergency situations involving a weapon or imminent risk of harm to self or others, a traditional emergency response is dispatched, which includes NYPD officers and an ambulance.
New Yorkers experiencing or witnessing an emergency should continue to call 911 for themselves, a loved one, a neighbor, or others.
When a B-HEARD Team is dispatched, the team arrives in an FDNY-branded vehicle and will have the same Basic Life Support equipment as an ambulance. Teams can be identified by their FDNY EMS uniforms and H+H identification. Callers cannot specifically request a B-HEARD Team. Based on a description of the circumstances, 911 operators will route the caller to speak with a trained EMT to triage and assign calls to B-HEARD based on the call location, dispatch criteria and availability of B-HEARD Teams.
B-HEARD is grounded in New York City's commitment to treat mental health emergencies as a health issue, not a public safety problem.
Before B-HEARD, NYPD officers and FDNY EMTs responded to nearly all mental health 911 calls; however, that often is not the most appropriate form of help for those experiencing a mental health emergency and lacks a mental health professional in the response. B-HEARD helps people with emergency mental health needs quickly get appropriate help and health-centered assessments from trained medical and mental health professionals.
The B-HEARD pilot has reduced unnecessary transports to hospitals, increased connection to ongoing mental health care and reduced the number of times police respond to 911 mental health calls. The results of this pilot will inform how the City responds to mental health emergencies in other neighborhoods.
B-HEARD Teams include two EMTs/paramedics and a mental health professional. As trained health professionals, the B-HEARD Teams can respond to a range of behavioral health problems, such as suicidal ideation, substance misuse, and mental health conditions, including serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. Team members bring significant experience with mental health crises and are trained jointly to use their physical and mental health expertise and experience in crisis response to assess and de-escalate emergency situations.
Once on the scene, the Team works with the person in need of assistance, and if appropriate, other involved parties. The Team uses their experience with crisis response to help de-escalate situations, if needed. They conduct physical and mental health assessments and can provide on-site assistance, including but not limited to connecting the person to their existing medical and/or mental health provider, crisis counseling, or, with their consent, connecting them to follow-up services. If the person requires emergency medical services, the B-HEARD Team provides emergency medical care and calls EMS for an ambulance transport.
Everyone served by B-HEARD is offered follow-up care. This can include help from a mobile crisis team, a Department of Homeless Services outreach team, or a hospital-based program. It can also include connecting or reconnecting clients to community-based healthcare or social service providers.
No. Callers cannot specifically request a B-HEARD Team. Based on a description of the circumstances and need, 911 operators and EMS are trained to triage and assign calls to B-HEARD Teams based on the call location, dispatch criteria and availability of B-HEARD Teams.
B-HEARD Teams will not be dispatched to 911 mental health calls where violence and/or imminent harm is identified by the 911 operator. Such calls will continue to be handled by NYPD and EMS. Once on the scene, NYPD or EMS can request support from B-HEARD Teams.
B-HEARD is an option for ages 6+ and B-HEARD responds to 911 calls from schools.
B-HEARD Teams respond to all mental health emergency calls without law enforcement with a few exceptions where there is increased risk for harm, including situations on subway tracks or involving weapons, imminent harm (as identified by 911 caller), crime in progress, or other circumstances requiring law enforcement assistance.
Once a B-HEARD Team has arrived at a location, they can request backup from NYPD if it is not safe for the B-HEARD Team to intervene.
In all neighborhoods other than the pilot neighborhoods, NYPD officers and FDNY/EMS EMTs will continue to provide coordinated responses to mental health emergencies. When there are no B-HEARD Teams available in the pilot neighborhoods, an ambulance and police officers will continue to respond.
B-HEARD Teams operate seven days a week, 16 hours a day in four of the five boroughs.
In Manhattan, B-HEARD covers Harlem (river to river), Washington Heights, Inwood
In the Bronx, B-HEARD now covers the entire borough.
In Brooklyn, B-HEARD covers East New York, Brownsville, East Flatbush, Remsen Village, Marine Park, Canarsie, Crown Heights, Wingate, and Prospect Lefferts
These areas were identified based on the volume of 911 mental health calls coming from these communities (these radio zones have among the highest volume of 911 calls in the city) as well as the availability of community-based mental health resources, such as Comprehensive Psychiatric Emergency Programs (CPEPs), outpatient clinics and other behavioral health providers.
B-HEARD represents a coordinated effort by FDNY/EMS and NYC Health + Hospitals, with oversight from the Mayor's Office of Community Mental Health, to move towards a more health-centered approach to mental health emergencies. FDNY EMS and H+H manage the B-HEARD Teams and provide training and ongoing support. The Mayor’s Office of Community Mental Health provides programmatic oversight for this pilot.
The key difference between B-HEARD Teams and other crisis responder programs are (1) when the teams intervene, (2) how quickly they arrive, and (3) the kinds of professionals who are on each team.
B-HEARD Teams respond to 911 mental health emergency calls within a comparable time as traditional EMS ambulance and include two EMTs/paramedics and a mental health professional, from FDNY/EMS and NYC Health + Hospitals.
Mobile Crisis Teams respond to referrals for urgent mental health crises and do not respond to 911 calls. From 8:00am to 8:00pm seven days a week, Mobile Crisis Teams arrive within hours to help people who are unable or unwilling to engage in care. Both responses involve face-to-face interventions with the identified individual in crisis, as well as their family or other support systems, to engage, assess, de-escalate and connect individuals to the most appropriate services. Most Mobile Crisis Teams include both professional and paraprofessional staff, for example, a master’s-level clinician with a peer support staff person. These teams consist of mental health clinicians and peers who can provide mental health services, primarily serving both children and adults in their homes. Mobile Crisis teams typically make between one and three contacts with the person in crisis over one to two weeks, provide crisis intervention, de-escalation, assessment and linkage to ongoing mental health and substance use treatment and support.
Providers making referrals to Mobile Crisis Teams for children and adults can select the Mobile Crisis Team Referrals option on the “For Providers tab” at nyc.gov/988.
Co-Response Teams (CRT) offer pre- and post-crisis intervention and do not respond to 911 calls. A collaboration between the NYPD and the Department of Health and Mental Hygiene, each team includes two police officers and a clinician, serving community members presenting with mental health or substance use challenges who are at an elevated risk of harm to themselves or others. CRTs offer short-term engagement to facilitate connections to care and linkages to support services. CRT officers volunteer for the assignment, and all CRT members have been trained in Crisis Intervention Training (CIT) and are skilled in working with community members presenting with mental health and substance use challenges.
An emergency is a situation that requires an immediate in-person response from first responders. If someone is at immediate risk of hurting themself or someone else or is in imminent danger because of a health condition or other situation, call 911 immediately.
Beyond 911, New York City also offers other options for people experiencing behavioral health crises. A behavioral health crisis is defined as a non-life-threatening situation in which a person experiences an intense behavioral, emotional, or psychiatric response that may be triggered by a precipitating event. The person may be at risk of harm to themself or others, disoriented or out of touch with reality, functionally compromised, or otherwise agitated and unable to be calmed; and if this crisis is left untreated it could result in an emergency.
Call 988. NYC 988 is your connection to free, confidential mental health support in a crisis that does not need an immediate in-person response. Speak to a counselor via phone, text, or chat and get access to mental health and substance use services, in more than 200 languages, 24/7/365. If you're not sure if 911 or 988 is more appropriate, contact 988 and a trained counselor will help to assess the most appropriate next steps, including connection to 911 or the City's full array of urgent mental health services. NYC 988 is your connection to get the help you need.
Search our database for behavioral health and substance use services that work for you.
Text-to-911 is a reliable and safe way to reach emergency services in New York City. You should always call 911 if you can and text 911 only if you can’t call. Text-to-911 is beneficial to the Deaf, people with hearing loss or speech disabilities, and those who can't safely call 911, including those experiencing domestic or intimate partner violence. For more information, go to https://www1.nyc.gov/site/text911/index.page.
