From Innovation to Integration
We are committed to finding what works. And when we find it, we ensure it becomes a lasting part of how our City government serves New Yorkers.
Every year, more than one out of every five adults in New York City experiences mental illness. That’s roughly equivalent to the number of people who live in Manhattan. People of all ages, backgrounds and status are affected by mental health challenges each year. Yet, for decades, hundreds of thousands of our fellow New Yorkers have gone without the care they need due to various barriers, including limited affordability and accessibility of services, a shortage of culturally responsive providers, language and informational gaps, and personal or cultural values that affects help-seeking. OCMH has worked to develop programs across City Agencies to help ensure every New Yorker with mental health needs has access to support.
FROM INNOVATION TO INTEGRATION
OCMH has worked to develop programs across agencies to ensure that every New Yorker has access to the mental health support that they need. These innovative programs, now fully integrated into City Agency operations, represent a historic investment in providing mental health services in places where New Yorkers are.
Assertive Community Treatment (ACT)
City implementation partner: Department of Health and Mental Hygiene (DOHMH)

Elmhurst Assertive Community Treatment (ACT) Team
Program description: Assertive Community Treatment (ACT) teams include mental health and substance use professionals and, at times, peer specialists. ACT teams typically meet with clients six times per month in their home or community to provide long-term behavioral health treatment, including medication. In 2016, ThriveNYC added a master’s level Substance Use Specialist to 40 ACT teams, enhancing these teams’ ability to serve people with co-occurring disorders. At any given time, ACT teams that receive partial funding from the Mayor’s Office of Community Mental Health have the capacity to serve 2,720 clients.
Need: About 43% of psychiatric hospitalizations in New York City in 2013 also indicated a co-occurring substance use disorder [Source].
Evidence: A study of one mobile treatment team in New York State that integrates criminal justice, healthcare, and community support services for individuals with severe mental disorders found a number of positive outcomes for participants, including significant reductions in arrests, incarcerations and jail days, and hospitalizations and hospital days [Source]. ACT teams that include substance use specialists have been shown to support significant improvements in mental health symptoms and residential stability among adults with a history of chronic homelessness and co-occurring mental health and substance use disorders [Source].
Reach and impact data highlights:
- Among clients discharged from the program in FY2021 Q2 after receiving ongoing care from a team, 33% had experienced incidents of homelessness in the six months prior to admission. This percentage dropped to 19% in the six months prior to discharge, while being served by a team (Assertive Community Treatment (ACT) Teams/Forensic Assertive Community Treatment (FACT) Teams/Shelter-partnered ACT Teams)
- Among clients discharged from the program in FY2021 Q2 after receiving ongoing care from a team, 61% had experienced incidents of psychiatric hospitalization in the six months prior to admission. This percentage dropped to 34% in the six months prior to discharge, while being served by a team (Assertive Community Treatment (ACT) Teams/Forensic Assertive Community Treatment (FACT) Teams/Shelter-partnered ACT Teams)
Assisted Outpatient Treatment (AOT) Coordination
City implementation partner: Department of Health and Mental Hygiene (DOHMH)

Derrick Brown works as a Peer Specialist on an Intensive Mobile Treatment team. Approximately 80% of people currently on AOT court orders are mandated to receive mobile mental health treatment.
Program description: Assisted Outpatient Treatment (AOT), commonly referred to as Kendra’s Law, is court-ordered mental health treatment and care coordination for people with a history of lack of compliance with treatment for mental illness. To enhance the City’s capacity to implement this important program, ThriveNYC added 20 staff to the Office of Assisted Outpatient Treatment.
Evidence: A 2009 independent evaluation of New York State’s AOT program found a significant reduction of roughly 25% in hospital admissions during the six months after an AOT court order, as compared to the pre-AOT time period. AOT clients also experienced a number of other improved outcomes, including: reduced hospital length of stay, increased receipt of psychotropic medication, and greater engagement in outpatient services [Source].
Reach and impact data highlights:
- 1,818 people were monitored by the AOT program in FY2021 Q2
- 51.4% of individuals no longer needed AOT because they were likely to engage in treatment voluntarily or survive safely in the community without court ordered treatment as evidenced by their adherence during AOT order and their presentation at a psychiatric exam in FY2021 Q2 (Oct 1, 2020-Dec 31, 2020)
Featured announcements:
Behavioral Health Assessment and Support for Young Adults in Detention
City implementation partner: Health + Hospitals / Correctional Health Services

Group mandala created by women in Mental Observation Unit with Merrill Cox, Licensed Creative Arts Therapist/Instructor - Correctional Health Services - 2020 creative arts therapy during COVID-19
Program description: Young adults who experience jail incarceration are disproportionately vulnerable to mental illness, substance misuse, and victimization compared with young adults who do not experience incarceration. To enhance support for these young people, our office supported 30 NYC Health + Hospital/Correctional Health Services (CHS) staff who conduct voluntary behavioral health screenings, substance use engagement, and therapeutic creative arts programming. The data for this program focuses on 18-to-21-year-olds (“young adults”) who are incarcerated on Rikers Island or in a borough-based jail for at least 7 days and are brought by the Department of Correction to CHS for screening. Screening data reported for this program do not include incarcerated young adults already in care of CHS’s mental health service. Prior to October 1, 2020, data for this program also included those 16- and 17-year-olds who were brought by the Administration for Children’s Services (ACS) to CHS for screening; now, ACS is implementing a separate program to address their behavioral health needs.
Need: According to a study by the Vera Institute of Justice, about 85% of young people assessed in secure detention reported at intake at least one traumatic event, including sexual and physical abuse and domestic or intimate partner violence. One in three young people screened positive for PTSD and/or depression [Source].
Evidence: A 2016 review of existing literature found that arts-based programming for justice-involved youth has positive effects on social and emotional development outcomes [Source].
Reach and impact data highlights:
- 6,215 creative arts therapy sessions were conducted through this program between 12/1/16 and 3/31/2021
- 1,550 youth and young adults were screened for behavioral health needs through this program between 11/01/2018 and 03/31/2021 (data collected FY20 onward includes only those who stayed at least 7 days)
- 91% of creative arts therapy participants surveyed between 10/01/2020 and 12/31/2020 reported that participating in the program helped them express their feelings
Featured publication: Creative Arts Therapy During COVID-19
Be Well: Mental Health Support for City Employees
City implementation partner: Mayor's Office of Labor Relations (OLR)

Program description: Be Well is a program of the Mayor’s Office of Labor Relations’ WorkWell NYC initiative that offers programs and resources to promote mental health among the 380,000 people employed by New York City. This initiative aims to create work environments that support the mental and emotional well-being of employees and create opportunities for employees to build resilience.
Need: One in five New Yorkers experiences mental illness in a given year [Source]. As the largest employer in New York City with over 380,000 employees [Source], the City has a critical opportunity to promote mental health for its employees.
Evidence: Characteristics of the most effective workplace mental health interventions include providing activities that address both mental and physical health, and support accessing clinical treatment and navigating disability management programs, among others [Source].
Reach and impact data highlights: 13,606 City employees participated in all Be Well activities between 7/01/2019 and 6/30/2020
Central Crisis Support Team (CCST)
City implementation partner: Department of Education
Program Description:
The Central Crisis Support Team (CCST) consists of licensed social workers and supervisors supporting New York City Public Schools with evidence-based practices, crisis intervention and preventive mental health supports, professional learning, educational and career pathways, and community-based partnerships. Formerly CSRCs, the CCST deploys a team of social workers to support schools and district offices during a crisis, thereby ensuring an immediate response. CCST evolved from deploying social workers to also offering professional training. Professional learning offerings are led with a culturally responsive lens, covering areas from social-emotional learning, mental health wellness, promoting student voices, building inclusive school communities, and caregiver engagement. NYC DOE is a NYS Department of Education Board for Social Work approved provider of continuing education credits for NYS licensed social workers, elevating professional growth. The CCST aims to provide students with a safe, secure, and supportive educational experience to promote social and emotional wellness that supports learning.
CCST social workers have provided services to nearly 500 students during the 2022/2023 school year and 95% of participants who engaged in professional learnings offered by the CCST reported moderate to high levels of competency using skills learned.
Need:
A 2021 survey that collected responses from more than 1,300 young people (ages 14 to 24) across New York City, with a representative share from all five boroughs, reported that more than a third (35%) of youth respondents wanted or needed mental health services from a professional, particularly amongst youth in the Bronx and Manhattan and among the youth who wanted or needed mental health services, only 42% reported receiving these services.1 Even before the pandemic, nearly 40% of New York City high schoolers reported feeling sad or hopeless every day for more than two weeks.2 Youth and families that are part of BIPOC communities are exposed to circumstances that lead to greater risk. In 2019, more Black (10.2%) and Latinx (9.4%) NYC high school students reported having attempted suicide within the past 12 months than White students (5.8%).326 A recent report found that suicide is the second leading cause of death for NYC adolescents ages 15-19 and the third leading cause of death among NYC children ages 5-14.274
Sources:
1 Voicing our future: Surveying youth on their priorities for 2021 and Beyond. CCC New York. (2021, June 21). Retrieved January 27, 2023, from https://cccnewyork.org/voicing-our-future-surveying-youth-on-their-priorities-for-2021-and-beyond/
2 2021 New York City Department of Health Youth Behavioral Risk Survey, New York City High School Survey Results. (n.d.). Retrieved From https://nyc.gov/assets/doh/downloads/pdf/episrv/codebook-citywide-yrbs-2019.pdf
3 2019 New York City Department of Health Youth Behavioral Risk Survey, New York City High School Survey Results. (n.d.). Retrieved From https://nyc.gov/assets/doh/downloads/pdf/episrv/codebook-citywide-yrbs-2019.pdf
4 CCC 2021-2022 annual report. CCC New York. (2022, December 16). Retrieved January 27, 2023, from https://cccnewyork.org/data-publications/ccc-2021-2022-annual-report/
Centralized Mental Health Services for Youth and Young Adults
City implementation partner: Department of Youth & Community Development (DYCD)
Program Description:
The Centralized Mental Health Services for Youth and Young Adults Program consists of eight mental health “hubs” located in all five boroughs and situated in DYCD’s Runaway and Homeless Youth drop-in centers. RHY drop-in centers offer a variety of services to youth ages 14 to 24 who run away, are experiencing homelessness, or are otherwise at risk and vulnerable. Each hub is equipped with experienced behavioral health professionals who are certified and trained to administer screenings and facilitate group and individual therapy to youth. The program provides much needed mental health services to youth who deal with traumatic circumstances and uncertainty or may otherwise benefit from behavioral health support and provides for a continuum of care at a centralized location. RHY drop-in centers and transitional living facilities can refer youth to the hubs for services.
REACH
Eight mental health hubs located in DYCD drop-in centers offer mental health services for youth ages 14-24. In FY 23, 518 young people enrolled in therapy at the hubs.
NEED
Youth experiencing homelessness in NYC are disproportionately youth of color (95%); gay, lesbian, bisexual, or queer/questioning (42%); and transgender/gender non-binary (8%). Source.
Mental health problems including depression, PTSD, and suicidal ideation are considerably more prevalent in youth experiencing homelessness than adolescents from the general population. Source.
Clinicians in Older Adult Centers
City implementation partner: Department for the Aging
Program Description:
Older adults have high rates of late-onset mental health disorders, yet low rates of assessment and treatment. To meet the needs of this population, the Department for the Aging placed clinicians at senior centers across the city to assess aging New Yorkers for mental health conditions and provide direct treatment as needed. Clinicians offer engagement activities as well as individual and group-based therapy sessions for those who screen positive for mental health conditions.
REACH
3,995 older adults have been assessed by mental health clinicians since this program began in 2016
NEED
85,000 seniors in New York City, or 9.4% of the City’s older adults, suffered from depression in 2017. Source
Less than 25% of older adults with mental illness currently receive treatment from mental health professionals. Source
Communities Thrive
City implementation partner: NYC Health + Hospitals
Program Description:
Communities Thrive aims to support communities of color in shaping how and where mental health support is delivered and in exploring new ways to address longstanding barriers to care. Studies show that locating mental health support in culturally responsive, community-based organizations and healthcare providers can mitigate barriers to care. In partnership with organizations serving Latinx New Yorkers, Communities Thrive will expand access to mental health care through community partnerships and connection to tele-mental healthcare provided by Health + Hospitals Corporation. The program plans to provide access to mental health care for up to 1,000 members of the Latinx community residing in under-resourced and low-income neighborhoods.
NEED
New Yorkers of color face a higher risk for mental health needs while receiving less mental health care than white New Yorkers. A serious shortage of mental healthcare providers – including too few culturally-responsive and multilingual clinicians, lack of insurance, and stigma all contribute to inadequate and unequal access to mental healthcare.
Latinx New Yorkers display higher rates of depression (12%) than white New Yorkers (8%) and are less likely to engage in treatment. Source.
Continuous Engagement between Community and Clinic Treatment (CONNECT)
City implementation partner: Department of Health and Mental Hygiene
Program description:
The city will launch a demonstration project, known as Continuous Engagement between Community and Clinic Treatment Teams (CONNECT), to enhance the capacity of existing clinics to provide a more flexible and nimble treatment model that not only addresses clients’ mental health needs but also their social and physical needs. This program aims to center communities by enhancing the mobile capacity of clinics based in communities most in need as determined by the current waitlist for mobile treatment services.
REACH
The CONNECT program provided services to 1,029 unique individuals in the clinic and in the community in the first quarter of FY2023.
Connections to Care: Mental Health Integration in Community-Based Organizations
City implementation partner: Mayor’s Office for Economic Opportunity
Employees of the Arab American Association of New York, part of Connections to Care, support community members in southern Brooklyn
Program description: Connections to Care (C2C) integrated mental health support into the work of community-based organizations (CBOs) serving at-risk and low-income communities across the City. Through C2C, CBOs that had not been providing mental health services worked with mental health providers who trained and coached staff to screen their clients for mental health needs, offer direct support when appropriate, and link to local health providers for further care if needed. This program was operated in partnership with the Department of Health and Mental Hygiene, with additional funding through the Mayor’s Fund to Advance New York City.
Update: In the summer of 2021, Connections to Care will be integrated into Jobs Plus, a program operated by the NYC Department of Social Services/Human Resources Administration that provides career training and employment services, with the goal of creating pathways to employment for public housing residents. By adding mental health services to the Jobs Plus program via the Connections to Care initiative (C2C), the City aims to increase clients’ ability to overcome barriers to employment that may be the result of unaddressed mental health challenges and achieve other targeted program-specific outcomes in areas such as job placement and financial independence.
In April 2021, the City announced a new partnership with the CUNY School of Professional Studies to create a Community Behavioral Health Academy that will train more than 5,000 City agency staff and social service providers in three years to better support the mental health of the people they serve. Drawing on the framework of task sharing, and building on the promise of Connections to Care (C2C) and other initiatives, the Academy will equip providers and City agencies with tools and resources to address and promote mental health.
Need: About 30% of the total population of New York City (or around 2.6 million people) resides in federally designated mental health professional shortage areas [Source]. Research has robustly and consistently shown that identities with a history of oppression – such as people of color – among others, experience increased negative mental health symptoms related to experiencing discrimination and harassment. [Source]. C2C provides people the opportunity to access mental health services in places where they are already going for other basic needs. Screening data from Connections to Care reveals that about 1/3 of CBO participants experience mental health symptoms, higher than the prevalence of symptoms in the wider population. (Program data collected by DOHMH/NYC Opportunity)
Evidence: The RAND Corporation led an independent evaluation of C2C from 2016 through 2020, which found that CBOs were able to expand the skillsets of their staff to identify and address mental health needs and promote positive mental health. The evaluation also found a positive effect on mental health and social services outcomes for specific groups, including expecting parents and parents of young children and participants in youth development and workforce development programs [Source].
Reach and impact data highlights:
- 1,930 CBO staff have been trained and 49,786 participants received services through this program since this program began in 2016 through December 31, 2020
- 70.7% of CBO participants experienced a clinically significant improvement in symptoms of depression or anxiety within 12 weeks of an initial positive screen
Featured publications:
Connectivity Program
City implementation partner: NYC Health + Hospitals
Program Description:
During the early months of the pandemic, many behavioral health patients responded well to tele-mental health options as demonstrated by higher attendance and retention in treatment. And yet, limitations to access persist: many patients lack devices and data plans with sufficient coverage for both tele-mental health services and regular use. The Connectivity Program – a partnership between OCMH and NYC H+H – provides devices and data to connect behavioral health patients with obstacles to virtual care to tele-mental health services. The program aims to provide devices and data plans to 1,000 high-risk patients with limited connectivity, who were diagnosed with COVID-19, or who have chronic disease and high mental health needs.
REACH
93% of people continue their mental health treatment within 30 days of receiving a device, 87% within 90 days, and 84% within 120 days. 813 total phones have been distributed since July 2021, and the most common recipients are Black men aged 51-60 years old in Manhattan.
NEED
40% of New York City households do not have comprehensive connectivity, (a combination of home and mobile broadband), which means that 3.4 million residents are excluded, entirely or in part, from digital life. Source.
As tele-mental health options grow in acceptance and prevalence with the onset of the pandemic, evidence indicates that virtual support can address the stigma around seeking care and breaking down other barriers to care. Source.
Co-Response Teams
City implementation partner: Mayor’s Office of Criminal Justice (MOCJ)

Program Description:
City implementation partners: Department of Health and Mental Hygiene and the New York City Police Department
Co-Response Teams (CRT) are a collaboration between the NYPD and DOHMH. CRT is a pre- and post-crisis intervention. Each team includes two police officers and one behavioral health professional. These teams work 14 hours per day, 7 days per week, to serve community members presenting with mental health or substance use challenges who are at an elevated risk of harm to themselves or others. The teams offer short-term engagement to facilitate connections to care and linkages to support services.
REACH
Over 3,208 community members have been served through this program since it began in 2016
NEED
169,000 mental health emergency 911 calls were received by the NYPD in 2017. The majority (56%) of these calls result in the individual being transported to the hospital, highlighting the need for partnership between law enforcement and public health workers. Source
Crime Victim Assistance Program (CVAP)
City implementation partner: Mayor’s Office of Criminal Justice (MOCJ)
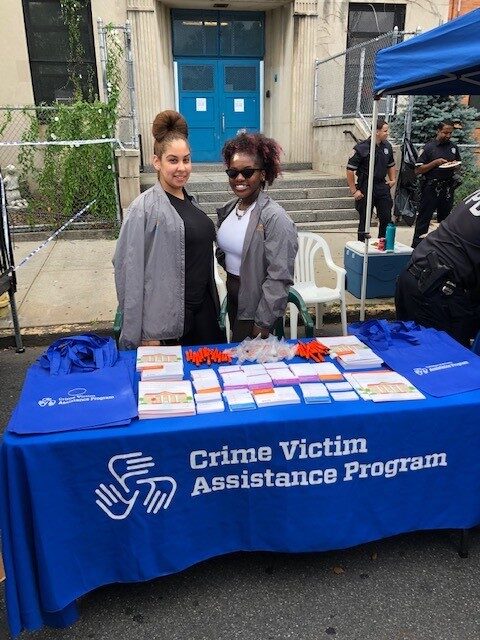
Program description: Victims of any kind of crime can be served by the Crime Victim Assistance Program, which operates in precincts and Housing Police Service Areas citywide. The program has dedicated victim advocates for survivors of domestic violence and additional advocates for victims of every other category of crime. The program provides safety planning and support in the immediate aftermath of a crime, as well as connections to ongoing individual or group therapy, and help navigating the legal and financial challenges that can emerge after a crime has occurred.
Need: 28%-45% of victims of violent crime suffer from PTSD, a condition which causes substantial distress, and can damage a victim’s education, employment, relationships, and physical health [Source]. 31% to 84% of women who have experienced intimate partner violence are estimated to experience PTSD [Source].
Evidence: One 2019 study found that 80% of victims of crime and violence who received any mental health support reported improved PTSD symptoms [Source]. A 2012 study found that intimate partner violence victims who received coordinated community response services were less likely to report PTSD, depression, and fear, and were more willing to leave their abuser than women in a comparison group [Source].
Reach and impact data highlights:
- Over 222,000 people have received support or services through this program since it began in 2016.
- 95% of victims report feeling safer physically and/or emotionally after receiving Crime Victim Assistance Program assistance
-
75% of victims served by the Crime Victim Assistance Program are BIPOC
Featured publications:
- Crime Victim Assistance Program: A survivor finds support
- Meet Yolanda McCray, Jailene Panarella, Crystal White, and Iris Wong, COVID-19 Mental Health Heroes from the Crime Victim Assistance Program
Crisis Intervention Training (CIT)
City implementation partner: New York City Police Department (NYPD)

Program description: Taught by Police Academy instructors and mental health experts, Crisis Intervention Training (CIT) helps NYPD officers better recognize and respond to the behaviors and symptoms of emotional distress and mental illness. The training includes role-playing, lectures, and conversations with individuals with mental illness who have had both positive and negative encounters with the police. The four-day training aims to increase officers’ skills in de-escalation of crises and improve the safety of both the officer and the individuals encountered.
Need: 10% of all law enforcement responses nationwide involve adults with untreated serious mental illness [Source].
Evidence: A 2017 systematic review of CIT programs has shown that CIT has positive associations with improved officers’ attitudes and knowledge about mental health, as well as on officers’ confidence in their ability to respond to individuals with mental illness [Source].
Reach and impact data highlights:
- 16,894 NYPD officers and staff were trained in CIT between 06/08/2015 and 3/31/2021
- 83% of trained officers surveyed in 2019 reported that they use the knowledge and skills gained from CIT
Early Childhood Mental Health Network (ECHMH)
City implementation partner: Department of Health and Mental Hygiene (DOHMH)

Program description: The Early Childhood Mental Health Network provides mental health support for young children and their families, helping to address challenges early. Mental health professionals consult with early childhood programs partnered with the Department of Education (DOE) to address program, classroom, and child-level challenges in order to strengthen the capacity of teachers and caregivers to support children. Seven early childhood therapeutic centers, open to all New York residents, located throughout the city offer specialized mental health treatment for children from birth to age five and their families, as well as access to family peer advocates and connection to ongoing support. Additionally, mental health professionals are able to receive specialized training in evidence-based practices and early childhood development through the Early Childhood Mental Health Training and Technical Assistance Center in order to increase the capacity and competencies of professionals working to identify and address the mental health needs of young children.
Need: 7% of children suffer from anxiety and 3% suffer from depression nationally. However, over 40% of children with anxiety and 20% of children with depression go without treatment [Source]. Infants, toddlers, and preschoolers may have significant mental health problems that have serious consequences for early learning, social competence, and lifelong physical health. Mental health is influenced by environments, experiences, and interventions. [Source].
Evidence: A recent meta-analysis of 36 controlled trials evaluating psychosocial treatment for over 3,000 young children found a large and sustained impact on early disruptive behavior problems (Comer et al., 2013). And additional review of 14 studies found that Early Childhood Mental Health Consultation is associated with reductions in teacher-reported externalizing behaviors. [Source] A 2016 randomized controlled trial found that children who received assistance and coaching from early childhood mental health consultants in Connecticut had significantly lower ratings of hyperactivity, restlessness, externalizing behaviors, and problem behaviors. [Source]
Reach and impact data highlights:
- 9,483 individuals participated in a training and 6,841 individuals participated in a mental health consultation since this program between July 1, 2016 and June 30, 2021
- 54.5% of families referred to an Early Childhood Mental Health Network clinic by an early childhood program attended their first appointment between April 1 and June 30, 2021
Expansion of Clubhouses for People with Serious Mental Illness
City implementation partner: Department of Health and Mental Hygiene (DOHMH)
Program description: For thousands of New Yorkers experiencing serious mental illness, New York City’s Clubhouses offer supportive communities. Staff and member-run Clubhouses provide a place to connect with many different services including but not limited to social, education, employment, and case management supports. Clubhouse membership has been shown to reduce hospitalization, decrease criminal justice involvement, and improve long-term health and wellness.
Need: Around 280,000 adult New Yorkers have serious mental illness, such as diagnoses of schizophrenia or major depressive disorder accompanied by functional impairment. Too many are not connected to the support they want and need, and the COVID-19 pandemic has exacerbated needs and access challenges, particularly among people who are experiencing homelessness or have been impacted by the criminal justice system.
Evidence: The Clubhouse Model of Psychosocial Rehabilitation has been in existence for over 70 years, has worldwide presence, and has positively affected thousands of individuals diagnosed with serious mental illness (SMI) [Source]. Clubhouses are evidence-based models of psychiatric rehabilitation — one-stop places that help people with serious mental illness by providing:
- Peer support and lifelong friendships
- Structure and learning or improving hard and soft skills by doing meaningful activities
- Access to services
- Supported employment and education support
- Socialization and recreation in a safe, restorative and structured setting
Clubhouses have shown their effectiveness regarding employment, quality of life and hospitalization. Indeed, several studies compare Clubhouses with other mental health programs. The results have demonstrated that Clubhouse members: find more salaried work, find jobs of higher quality, have a better quality of life and face fewer hospitalizations compared to people in other psychosocial rehabilitation programs [Source]. Additionally, research shows that the Clubhouse model reduces hospitalization and justice involvement and improves health and wellness.
Reach and impact data highlights:
- Clubhouse members and staff conducted outreach and enrollment activities citywide at sites such as soup kitchens, pantries, shelters, justice-related settings, and hospitals.
- Since launching the expansion initiative in July 2021, almost 1,200 additional individuals with serious mental illness joined Clubhouse programs.
Forensic Assertive Community Treatment (FACT)
City implementation partner: Department of Health and Mental Hygiene (DOHMH)

Program description:
Forensic Assertive Community Treatment (FACT) teams provide ongoing, community-based mental health treatment and other supportive services to people living with a serious mental illness who have experienced a recent interaction with the criminal justice system. These multi-disciplinary teams aim to improve the quality of life for clients though treatment, rehabilitation, housing support, and a full range of community services. FACT teams have a capacity to serve 340 clients at any given time.
Need:
33% of women and 15% of men re-entering the community after incarceration have been diagnosed with a mental illness [Source].
Evidence:
A 2017 randomized controlled trial of a FACT program in New York State found that, on average, FACT participants had significantly fewer convictions, days in jail, and days in the hospital, and significantly more days in outpatient treatment [Source]. A study of one mobile treatment team in New York State that integrates criminal justice, healthcare, and community support services for individuals with severe mental disorders found a number of positive outcomes for participants, including significant reductions in arrests, incarcerations and jail days, and hospitalizations and hospital days [Source].
Reach and impact data highlights:
- Among clients discharged from the program in FY2021 Q2 after receiving ongoing care from a team, 33% had experienced incidents of homelessness in the six months prior to admission. This percentage dropped to 19% in the six months prior to discharge, while being served by a team (Assertive Community Treatment (ACT) Teams/Forensic Assertive Community Treatment (FACT) Teams/Shelter-partnered ACT Teams)
- Among clients discharged from the program in FY2021 Q2 after receiving ongoing care from a team, 61% had experienced incidents of psychiatric hospitalization in the six months prior to admission. This percentage dropped to 34% in the six months prior to discharge, while being served by a team (Assertive Community Treatment (ACT) Teams/Forensic Assertive Community Treatment (FACT) Teams/Shelter-partnered ACT Teams)
Featured announcements: A recovery for all of us: Mayor de Blasio announces new programs to support New Yorkers experiencing serious mental illness, April 28, 2021
Health Engagement and Assessment Teams 911 Follow Up (HEAT)
City implementation partner: Department of Health and Mental Hygiene and Fire Department Bureau of Emergency Medical Services
Program Description:
Health Engagement and Assessment Teams (HEAT), comprised of a behavioral health professional and a peer, is a time-limited case management intervention initially launched in late 2018 geared towards individuals exhibiting health or behavioral health needs that can benefit from peer engagement and support. The program is designed to help individuals remain connected to their communities and assist them in obtaining the care and services they need to remain healthy. The expansion of HEAT allows the Department of Health and Mental Hygiene to extend its services to people served by the Behavioral Health Emergency Assistance Response Division (B-HEARD), as needed, including follow-up care for everyone who is served by B-HEARD in their homes. The expansion also allows HEAT to proactively engage New Yorkers who most frequently call 911 and are transported to a hospital by the Fire Department (FDNY) Bureau of Emergency Medical Services (EMS).
REACH
HEAT teams served 224 unique individuals referred by FDNY 911 EMS and B-HEARD in FY22.
NEED
586 unique New Yorkers required 911-EMS response and transport to a hospital more than 3 times in a single month in a May 2021 analysis by FDNY.
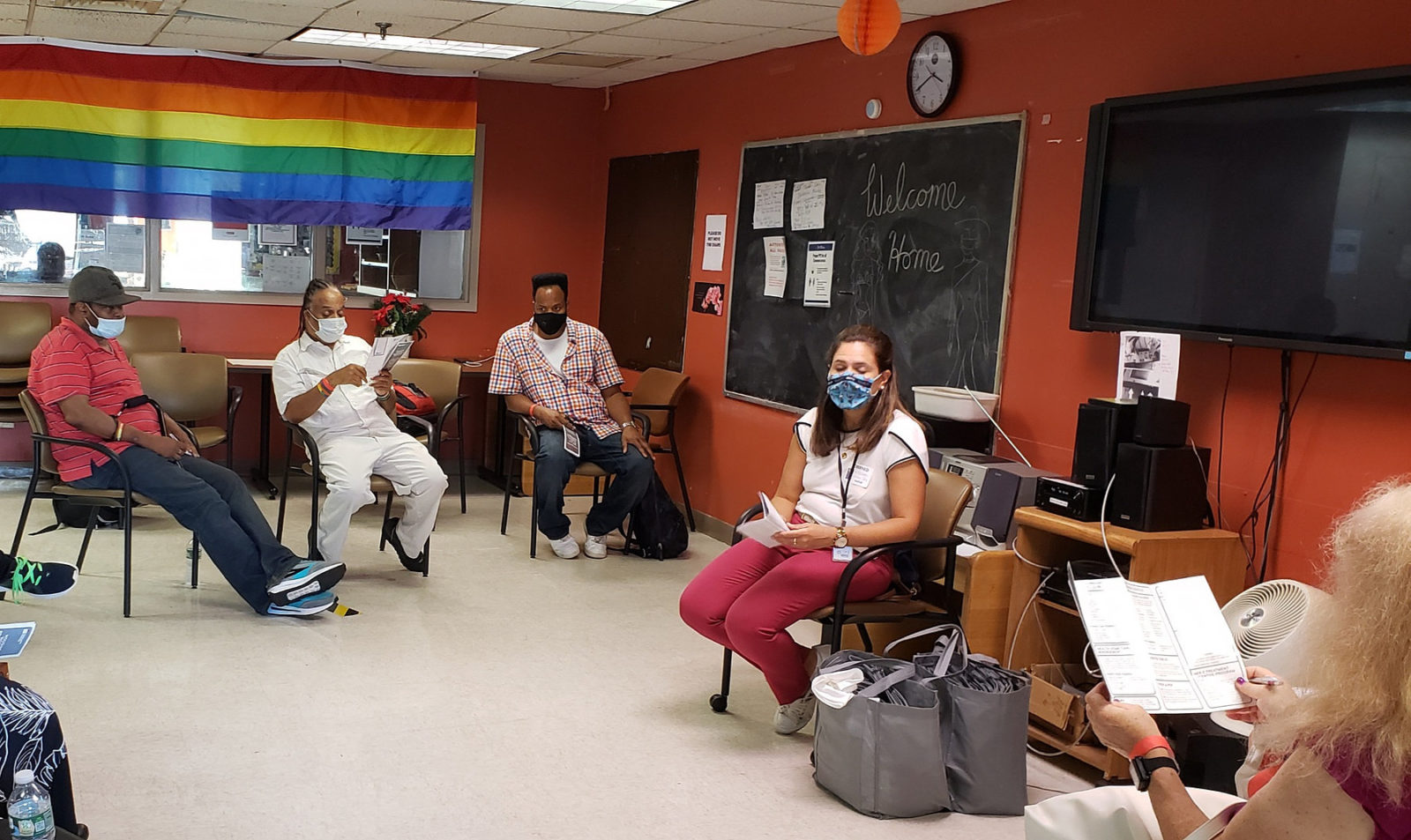
Intensive Mobile Treatment (IMT) Teams
City implementation partner: Department of Health and Mental Hygiene (DOHMH)

Program Description:
Intensive Mobile Treatment (IMT) teams provide intensive and continuous support and treatment to individuals right in their communities, where and when they need it. Clients have had recent and frequent contact with the mental health, criminal justice, and homeless services systems, recent behavior that is unsafe and escalating and were poorly served by traditional treatment models. IMT teams include mental health, substance use, and peer specialists who provide support and treatment including medication and facilitate connections to housing and additional supportive services.
REACH
837
clients can be served by IMT teams in New York City at any given time
NEED
The 800 individuals most frequently admitted to New York City jails in 2013 were more likely to have serious mental illness: 19% vs. 8.5% in a comparison group. Source
These 800 individuals are also more likely to have experienced homelessness (51.5% vs. 14.7%) and reported substance use (96.9% vs. 55.6%) than a comparison group. Source
Mental Health First Aid (MHFA)
City implementation partner: Department of Health and Mental Hygiene (DOHMH)

Program description: Mental Health First Aid (MHFA) is an evidence-driven, free, eight-hour training that, prior to the COVID-19 pandemic, was regularly provided seven days a week in all five boroughs to expand the number of people who can help New Yorkers in need. Conducted in English, Mandarin and Spanish, MHFA helped trainees recognize mental health needs, learn how to talk about them, and learn where to direct people in need to ongoing care.
Update: In June 2020, Mayor Bill de Blasio announced – as part of the Task Force on Racial Inclusion and Equity - that DOHMH would re-direct Mental Health First Aid (MHFA) staff to communities hit hardest by the pandemic for a Community Conversations initiative focusing on Mental Health, Equity & Resilience. This program holds structured discussions with communities about the impact of the pandemic, including structural racism, providing coping and resiliency skills, and informing residents of available mental health resources.
Need: The stigma associated with mental health challenges has been shown to have a direct relationship to lower levels of help-seeking behaviors [Source]. Stigma also has a strong relationship to lower levels of hope and self-esteem, increases the severity of psychiatric symptoms, and lowers the likelihood of staying connected to treatment [Source].
Evidence: MHFA has been shown in numerous studies to affect trainees’ knowledge, behaviors and attitudes towards mental health, including recognition of mental disorders, beliefs about effective treatment, and confidence helping others around mental health [Source].
Reach and impact data highlights: 159,952 individuals were trained in MHFA between 12/01/2015 and 06/30/2020
Featured announcements: Mayor de Blasio and Taskforce on Racial Inclusion & Equity Announce Expansion of NYC Care and Mental Health Services to Address Disparate Impact of COVID-19 on People of Color, June 9, 2020
Mental Health Outreach and Support for Veterans
City implementation partner: Department of Veterans' Services (DVS)

Program Description:
New York City is home to over 210,000 veterans, some of whom experience symptoms of post-traumatic stress disorder or major depression. To enhance mental health support for veterans, dedicated care coordinators worked directly with veterans to connect them to a range of community-based services as they transition home. These teams also engaged and offered support to veterans’ families and caretakers.
Need:
210,000 veterans live in New York City. 11% of these individuals were deployed after 9/11. [Source] 20% of veteran and service members of the Iraq or Afghanistan wars living in New York State suffer from either PTSD or major depression. About half of those in need of treatment seek help; however only half of those receive minimally adequate care [Source].
Evidence:
A 2016 study showed that Washington State veterans who had connected to outreach services were three times more likely to schedule an intake appointment, attend their appointment, and enroll in treatment than those who had not [Source].
Reach and impact data highlights:
11,500+ veterans, military families, and caregivers accessed services and support through this program between 2017 and 2021
Mental Health Service Corps
City implementation partner: NYC Health + Hospitals
Program Description:
The Mental Health Service Corps (MHSC) is a workforce development program that aims to build a diverse generation of mental health clinicians, equipped to integrate behavioral health into a variety of settings including primary care, women’s health, pediatrics, and other non-behavioral health care settings. Early-career clinicians receive intensive training in evidence-based practices and are placed throughout the NYC Health + Hospitals system with the goal of emerging from the three-year program seasoned and adept clinicians. Under the supervision of licensed clinicians, this intensive and innovative training experience will allow Corps Members to work effectively within interdisciplinary teams and be prepared to screen, assess, and treat patients in a culturally competent manner.
REACH
14,204 individuals received clinical services from Mental Health Service Corps behavioral health clinicians since data collection began on 01/01/2020
NEED
17 areas within New York City are currently federally designated as mental health provider shortage areas. Source
Mental Health Services for High-Needs Schools
City implementation partner: Department of Education (DOE), Department of Health and Mental Hygiene (DOHMH)

Program description: Symptoms of mental health conditions frequently emerge before the age of 14. The Office of School Health implemented new mental health services at 173 high-needs schools serving grades K through 12. Participating schools have on-site clinical services, including group and individual counseling for students, to integrate mental health services in school settings, improve the mental health outcomes of students, and build schools’ capacities to address the mental health needs of their school communities. This program began in fall 2017.
Need: 32% of New York City students report feeling sad or hopeless for at least a two week period in the past twelve months. Nearly 270,000 five- through 17-year olds in New York City are believed to have a diagnosable mental disorder; 134,000 of whose symptoms are severe enough to impact their daily functioning [Source].
Evidence: A recent study found that students in schools who received on-site mental health clinicians to identify and treat children with mental health needs demonstrated a significantly greater increase in prosocial behavior (as rated by both parents and teachers) than students who did not [Source]. An additional study of four school-based mental health programs that provided on-site clinical services found that all four programs decreased the percentage of youth in the clinical range on a scale of emotional functioning [Source].
Reach and impact data highlights:
- Students participated in 201,298 individual or group supportive counseling sessions since this program began in 2017 through December 31, 2020
- 16,478 trainings have been provided to teachers, staff, and families since this program began in 2017 through December 31, 2020
Mental Health Services in Domestic Violence Shelters
City implementation partner: HRA/DSS, Mayor’s Office to End Domestic and Gender based Violence, NYC Health + Hospitals

Program description:
This program is a collaboration between HRA/DSS, Mayor’s Office of Community Mental Health, Mayor’s Office to End Domestic and Gender based Violence and NYC Health + Hospitals. Through this program, multidisciplinary teams of mental health professionals will provide culturally competent, domestic violence-informed care and treatment to children, teens, and adults in the 55 domestic violence shelters across NYC. Services provided on-site and via telehealth also include crisis support for individuals and families as well as training and support for staff.
REACH
9,439 adults and children received domestic violence residential services in 2020. This service will be available and accessible to all shelter residents. The actual number of those who receive clinical services will be reported once the program is fully operational.
NEED
30% of adult women who experience intimate partner violence reported “serious psychological distress,” and 31% to 84% of women who have experienced intimate partner violence are estimated to experience PTSD and other problems including depression and higher rates of substance use. Source.
There are serious mental health consequences for children who witness and or experience domestic violence. Source.
Mental Health Services in Family Justice Centers
City implementation partner: Mayor’s Office to End Domestic and Gender-Based Violence

Program Description:
To bring mental health support to survivors of intimate partner violence, the Mayor’s Office to End Domestic and Gender-Based Violence partnered with NYC Health + Hospitals to add dedicated mental health teams to Family Justice Centers (FJCs). These new mental health teams provide direct on-site clinical services and complement the trauma-informed, comprehensive services available in each of the City’s five FJCs.
REACH
Over 1,516 clients have received mental health services at FJCs since this program began in 2016
NEED
About 30% of adult women who experience intimate partner violence reported “serious psychological distress,” much higher than the 7% prevalence amongst women who reported no experience of intimate partner violence. Source
Mental Health Services in Family Shelters
City implementation partner: Department of Homeless Services

Program Description:
Families experiencing homelessness often have multiple service needs – which can be easier to navigate with support from a behavioral health professional. The Mayor’s Office of Community Mental Health and DHS has placed Licensed Master Social Workers (LMSWs) or Licensed Mental Health Counselors (LMHCs) in family shelters to provide assessments to families and coordinate with other shelters' social service staff to better connect families to behavioral health and other services.
REACH
34,815 families were screened for behavioral health needs since this program began in 2016.
NEED
12,124 families, including 21,726 children, were in New York City’s shelter system as of December 2019. Source
Mental Health Services in Runaway and Homeless Youth Residences and Drop-In Centers
City implementation partner: Department of Youth and Community Development (DYCD)

Program description: Young people who are served by Runaway and Homeless Youth Residential and Drop-in Center programs may experience family rejection, neglect, abuse, or trauma. The providers that are contracted to operate Runaway and Homeless Youth Residential and Drop-in Centers hire mental health professionals to provide evaluations, on-site individual and group counseling, and connect young people to additional, longer-term mental health services if necessary.
Need: Youth experiencing homelessness in NYC are disproportionately youth of color (95%); gay, lesbian, bisexual, or queer/questioning (42%); and transgender/gender non-binary (8%) [Source].
Evidence: A 2009 systematic review of services and interventions in drop-in centers and shelters demonstrated short-term benefits to youth, such as reduced school and employment challenges at six weeks, and reduced substance abuse at discharge [Source].
Reach and impact data highlights:
- 16,445 youth participated in mental health services between July 1, 2016 and June 30, 2021
- 78% of youth reported that program services are supporting their mental well-being between April 1 and June 30. 2021
Mobile Crisis Teams Expansion
City implementation partner: Department of Health and Mental Hygiene (DOHMH)

Program Description:
Mobile Crisis Teams use face-to-face interventions in a non-emergency crisis to engage, assess, de-escalate, and connect individuals to the most appropriate services. Deployed through NYC Well or hospitals, teams connect children and adults to new providers in addition to reconnecting to pre-existing care. Linkages are made to mental health, substance use, peer services, and social services. Most MCTs include both clinical and peer staff – for example, a licensed social worker and a certified family peer advocate. OCMH partnered with DOHMH to enhance the capacity of the teams to respond quickly – now, from 8 am-8 pm, 7 days a week, MCTs can arrive at a location within two hours, down from an average of 17 hours in 2017.
REACH
24 mobile crisis teams now serve New Yorkers citywide and have responded to 10,738 referrals from NYC Well in FY22.
NEED
68% of mental health-related emergency department (ED) visits in New York City did not result in admission to the hospital, indicating that not all crises require hospitalization and may be addressed with community-based support. (2015 NYC Mental Health Needs Assessment).
Newborn Home Visiting Program in Shelters
City implementation partner: Department of Health and Mental Hygiene (DOHMH)
Program Description:
In partnership with the Mayor’s Office of Community Mental Health, the Newborn Home Visiting Program was expanded to serve families with newborns up to 2 months of age residing in Department of Homeless Services shelters. With services collaboratively implemented by a public health advisor and a social worker, families are offered three visits and one follow-up phone call over the course of eight weeks, during which a trained public health advisor provides health education, depression screenings, and resources to improve child development, secure attachment, bonding, breastfeeding, infant safe sleep and connects families to community resources. The public health advisor refers caregivers who could benefit, to mental health counseling provided by a Newborn Home Visiting Program social worker and DHS Clinical care Coordinator, (DHS) as well as connects caregivers to mental health services provided in the community.
REACH
Over 7,500 caregivers were screened for postpartum depression through this program since this program began in 2015.
NEED
Pregnant women experience increased mental health and health risks associated with homelessness.1 One in 10 mothers report experiencing symptoms of postpartum depression.2
SOURCES
- Clark, R. E., Weinreb, L., Flahive, J. M., & Seifert, R. W. (2019). Homelessness Contributes To Pregnancy Complications. Health affairs (Project Hope), 38(1), 139–146. https://doi.org/10.1377/hlthaff.2018.05156
- Prevalence of Selected Maternal and Child Health Indicators for New York State, Pregnancy Risk Assessment Monitoring System (PRAMS), 2016-2020 (cdc.gov)
NYC Well (now 988)
City implementation partner: Department of Health and Mental Hygiene (DOHMH)
Program Description:
NYC Well (now 988) provides a single point of entry to the City’s mental health and substance misuse services via comprehensive 24/7/365 support over the phone, through text messaging, or through online chat. NYC Well provides robust crisis counseling, referrals to ongoing care, help with scheduling appointments, connection to mobile crisis services, peer support, and follow-up. NYC Well works to connect people to appropriate services regardless of insurance or immigration status.
REACH
1,656,056 calls, texts, and chats have been answered by NYC Well between 10/24/2016 and 06/30/2022
NEED
18% of participants in a survey of over 1,000 NYC Well users noted they would not have contacted anyone in the absence of NYC Well. The same survey showed that approximately two-thirds of survey participants reported that their contact with NYC Well helped them a lot, and nearly 90% said it helped at least a little. Source
School Mental Health Specialists
City implementation partner: Department of Education (DOE) and the Department of Health and Mental Hygiene (DOHMH)
Program Description:
The School Mental Health Program (SMHP) is part of the Office of School Health (OSH). SMHP began in 2015. Since this time, SMHP staff work in direct collaboration with schools, mental health provider agencies, students, and families to support the mental health and social-emotional needs of students attending over 1,100 DOE public schools. In this capacity, SMHP Specialists worked across multiple school settings to provide educational workshops on mental health topics and help schools become more knowledgeable and accepting of mental health care.
In 2019, in partnership with the Office of Community Mental Health, the SMHP Specialists provided enhanced support to school staff and parents/caregivers with the social, emotional, and behavioral development of students. In addition to the work already happening, SMHP Specialists provided direct skills groups to address school needs after COVID-19. The program was restructured to provide more individual services to 300 schools and to expand the capacity to connect students to mental health support in their schools. Specialists also helped identify students who would benefit from trauma-focused group counseling and provided those students with a series of supportive, evidence-based counseling sessions.
Overall, the SMH program has now expanded program implementation, relationship management, and quality assurance of onsite mental health services in over 700 DOE schools. Those schools ensure adaptation and sustainability of access to services to address the mental health service needs of students through onsite mental health CBO partners. By ensuring access to the almost 400,000 students served, SMH provides hands-on technical assistance, training, and school-level needs assessment. SMH also develops multiple school-based mental health programs and initiatives and links schools to community-based mental health clinics.
NEED
82% of teachers reported an insufficient number of school mental health professionals as a barrier to supporting mental health needs in school settings. Source
EVIDENCE:
A study of evidence-based trauma intervention in schools found reductions in symptoms of post-traumatic stress and increases in child functioning. [Source]. Multitiered models of school-based mental health supports that include mental health promotion, psychoeducation, prevention, and treatment are recommended to meet the increasing mental health needs of school-aged children [Source]. School-based brief group interventions to treat child and adolescent anxiety and depression have yielded positive results [Source]. Specialists expanded children’s access to mental health promotion, prevention, and treatment by offering preventive services as well as skills based supportive group counseling in schools and by referring youth in need to community-based supports.
REACH:
- In the first 3 quarters of FY 2022, School Mental Health Specialists reached over 200 New York City Department of Education schools.
- During this time, School Mental Health Specialists enrolled 255 students in skills-based group supportive counseling. Eighty-five (85) students were referred to mental health treatment provided by community-based mental health organizations.
- 14,879 students participated in skills-based classroom supportive services facilitated by School Mental Health Specialists.
Social Emotional Learning (SEL)
City implementation partner: Department of Education (DOE)

Program description: Social, emotional, and behavioral regulation skills are foundational for learning and well-being. Through a partnership between the Mayor's Office of Community Mental Health and the Department of Education, Pre-K and 3-K programs across New York City provide social-emotional learning support to students, families, program leaders and teaching teams.
Need: 43% of children in New York State (0-17) had experienced adverse childhood events in their lifetime, a 2011-2012 survey found [Source]. Adults who had experienced childhood emotional, physical, or sexual abuse were four to twelve times more likely to experience alcoholism, drug abuse, depression, and suicide attempt, according to the Adverse Childhood Experiences Study (ACE Study) [Source].
Evidence: There is a consensus among scholars that schools provide a powerful opportunity to provide social and emotional learning [Source]. Enhancing school staff’s ability to conduct provide successful social and emotional programming through universal interventions can have significant positive effects on students’ social and emotional skills, attitudes, behavior, and academic performance [Source].
Reach and impact data highlights:
Over 3,000 schoolteachers and program staff participated in at least one professional learning session since the program launched in 2016
- More than 3,000 parents and caregivers have attended family workshops to learn social emotional development practices since 2016
- 91.4% of classroom staff reported that they learned one skill or strategy to help children manage their feelings or behaviors between January 1 and March 31, 2021
- 1,979 parents and caregivers participated in family support workshops or trainings between January 1 and March 31, 2021
Support and Connection Centers
(formerly Diversion Centers)
City implementation partner: Department of Health and Mental Hygiene (DOHMH)
Program Description:
New York City is pioneering two Support and Connection Centers to give first responders an alternative to avoidable emergency room visits or criminal justice interventions. The centers offer short-term clinical and non-clinical services to people with mental health and substance use needs and promote community-based and person-centered engagement, stabilization, and connection to services. Guests (defined as people who were referred to, eligible for, and chose to receive services at a Center) are offered mental health, medical, substance use, and peer support services; help with basic needs; and discharge planning. Length of stay varies from a few hours to a few days depending on the guest’s needs. The East Harlem Support and Connection Center opened in February 2020, suspended in-person operations from March to October 2020 due to the COVID-19 pandemic, and re-opened with modified services in late October 2020. In July 2022, the center began operating at full capacity and the second center opened in the Bronx with limited capacity.
REACH
81% of guests referred to ongoing support are successfully connected or reconnected to treatment or other services following their stay
NEED
169,000 mental health emergency 911 calls were received by the NYPD in 2017. The majority (56%) result in the individual being transported to the hospital, highlighting the need for partnership between law enforcement and public health workers. Source.
Visiting Program for Homebound Older Adults
City implementation partner: Department for the Aging (DFTA)

Program description: Homebound older adults are often at risk of profound social isolation and loneliness. The Mayor’s Office of Community Mental Health partnered with the Department for the Aging to implement a Visiting Program for Homebound Older Adults, in which trained volunteers visit homebound older adults in their homes and build lasting relationships. The program links people with compatible interests, and aims to reduce social isolation and loneliness and improve the overall quality of life for homebound older adults.
Need: 1 in 3 older adults in New York lives alone. [Source]
Evidence: A systematic review of programs addressing social isolation in older adults indicates that home visiting interventions may have benefits including social support, loneliness, and mental and physical health. [Source]
Reach and impact data highlights:
- 2,107 older adults were visited 112,451 times through this program between 07/01/2017 and 06/30/2021
- 64% of older adults receiving visits reported feeling less socially isolated six months after joining the program between April 1 and June 30, 2021









